Written by Dr Wolfgang Muller
Written 01/07/2021 – Last major review 22/11/2021 – Last minor review 01/11/2023 – Next mandatory review by Nov 2024
Click on subject in CONTENT to go straight there and click on subject in the TEXT to go back to CONTENT
Content
My child is always sick – this cannot be normal!
How many infections may be completely normal in children over one year?
Why does my child seem to be so different to other children?
Why is it normal that children between the age of 6 months and 5 years have so many infections?
If this is all normal then surely I do not have to worry at all?
What is the minimum workup my child should have if I am worried about frequent infections?
What can I do to make my child better?
What could be wrong with my child to make him/her get so many infections?
Overview of conditions contributing to recurrent infections
Environmental factors
Abnormalities of the lungs
Nutritional deficiencies
Recurrent viral induced wheeze and airborne triggers
Deficiencies of the immune system
Temporary lung conditions
Chronic lung conditions
There is hardly a week I am not asked this question in clinic or in the Emergency Department. Parents are understandably worried when their infant or toddler seems to be catching one infection after the other. No month seems to go by when they do not have a fever or cough or are unwell with what looks like an infection of some sort. Most commonly it is a constant cough which does not seem to shift or a fever that seems to return ‘like clockwork’. Others always have a runny nose or complain of their throat hurting on a regular bases.
Surely this is not normal – how could it be? In order to answer this one has to understand: What is actually normal?
Well first of all it depends on the age of the child!
The age group I typically see with recurrent infections are between 8 months and 5 years of age. Although typically the first infection starts around 6 months of age most infants have reached the age of 8 months by the time they had their ‘recurrent’ infections. Not uncommonly children get what is called ‘bronchiolitis’ even earlier than that and typically from 4-6 weeks onwards.
If your child is outside this age range you should see a doctor and I would most certainly investigate this further.
Between 6 months to 5 years children develop their immune system gradually and every child may respond very differently when exposed to viruses and bacteria.
Studies from London and around the world have demonstrated that a healthy child even without infections may cough on average 11 times on a single day but this can vary between 1 to 34 coughing episodes per day!(1)
Other studies looked at how many infection do occur in healthy children and found on average 3 to 6 but in some children (with no other medical condition) up to 12 infections in a single year. (2)(3)(4)
Many parents ask doctors and nurses: ‘how long should the cough last for?’. I have covered this also under “Acute viral illness – what can I do?” This is not easy to answer because it varies a lot. Studies found that most coughs last between 1 and 3 weeks.(5) An Australian group of doctors also found that 50% of children had stopped coughing after 10 days and 90% of the children by 25 days. However it is important to understand that 8% of the children had a cough lasting longer than 28 days.(6) Some children go on and develop a ‘habit cough’, which is covered under “Respiratory – Habit cough”.
I show the picture quite often to parents to demonstrate how many days in a year a perfectly healthy child could be ill (red boxes) if they get 12 infections each lasting 3 weeks!
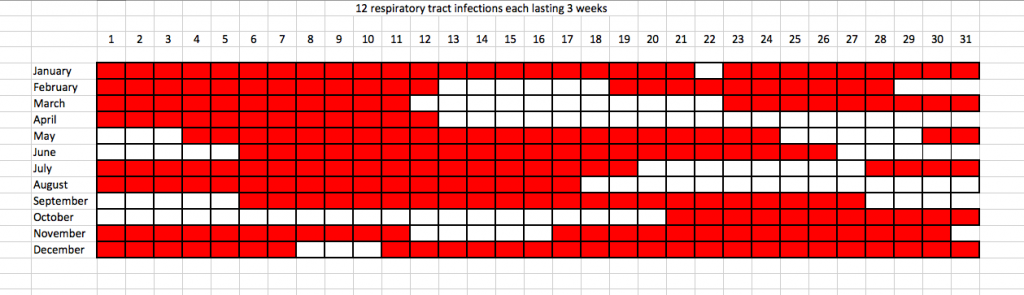
During the peak of the season it is not unusual to go from one infection straight into the next. This may be with a period of slight improvement before they are getting worse again or not even with any improvement in-between.
- Munyard, P. & Bush, A. How much coughing is normal? Arch. Dis. Child. 74, 531–534 (1996).
- Grüber, C. et al. History of respiratory infections in the first 12 yr among children from a birth cohort. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 19, 505–512 (2008).
- von Linstow, M.-L. et al. Acute respiratory symptoms and general illness during the first year of life: a population-based birth cohort study. Pediatr. Pulmonol. 43, 584–593 (2008).
- Bryant, P. A. & South, M. Fifteen-minute consultation: The infant with frequent infections. Arch. Dis. Child. Educ. Pract. Ed. 99, 8–12 (2014)
- Hay, A. D., Wilson, A., Fahey, T. & Peters, T. J. The duration of acute cough in pre-school children presenting to primary care: a prospective cohort study. Fam. Pract. 20, 696–705 (2003).
- Hay, A. D. & Wilson, A. D. The natural history of acute cough in children aged 0 to 4 years in primary care: a systematic review. Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 52, 401–409 (2002).

Why are not all children the same?
This is much easier to answer as we know well no two children are the same not even twins.
Some children are tall others small, heavier or lighter, better in sports, music or maths than others and so on.
So the same is true for our immune system. For some children the immune system learns to build up a defence with very little obvious symptoms while other children show a lot of symptoms. It is a little bit the same for adults. In medicine we have always known that some children and adults have no or hardly any symptoms when they have an infection while others are more likely to become quite ill with it before recovering. Although there are many factors contributing to that – one factor however is that our immune system deals with infections very differently from one person to another.
So yes, I also see great variation even within the same family and I have even seen this also to be true for twins: one sibling can be far more often sick than the other without any obvious reason.
As I mentioned it is a little bit like one may be taller and the other one a bit smaller.
…but overall your child is most likely not so different to many other children but you may not have come across it.
Probably almost all of us have come across a story of cases that have been missed for many months or even longer before they have been diagnosed. Sometimes it can be very late to treat this individual cases effectively. This is why I strongly recommend a careful review as this is key to minimise this risk. In most cases a careful history and examination without any additional tests gives me all I need to know. I have summarised somewhere else: “What is the minimum workup my child should have if I am worried about frequent infections?” and “Why does my child seem to be so different to other children?”
Not all cases are the same but also remember if your child is overall growing and developing normally there is time to explore whether there is actually something wrong with your child or not!
This is because the immune system has not yet developed fully.
Newborns get a ‘whole load’ of passive immunity called immunoglobulins from their mothers while they are still inside the womb (immunoglobulin G or IgG) and then some more if they are breast feeding (immunoglobulin A or IgA). The immunity at birth is mainly against viral infections but not so against bacterial infections. This is one reason why we do have to screen a small baby (first 3-6 months of life) very carefully for bacterial infections as soon as they develop a fever. Some infants also get protective antibodies mainly against viral gastrointestinal infections from breast milk, which also declines from 6-9 months.
So, in essence, babies do not have a protection from severe bacterial infections but almost the same protection as an adult from viral infections.
However, there is yet another twist, the immunity to viral infections wears off around 5-6 months and viral infections become more and more common.
After that children are “on their own” to develop immunity but have to come across that infection in the first instance. This process is most noticeable up to school age but developing immunity carries on lifelong!
I sometimes compare the situation of a small child with a young person who gets a one off ‘pocket money’ from their parents before they go out into the wider world to find a regular income without the support from their parents. The pocket money wears off around 6 months and then they may go through a hardship with little money until they find a regular income…
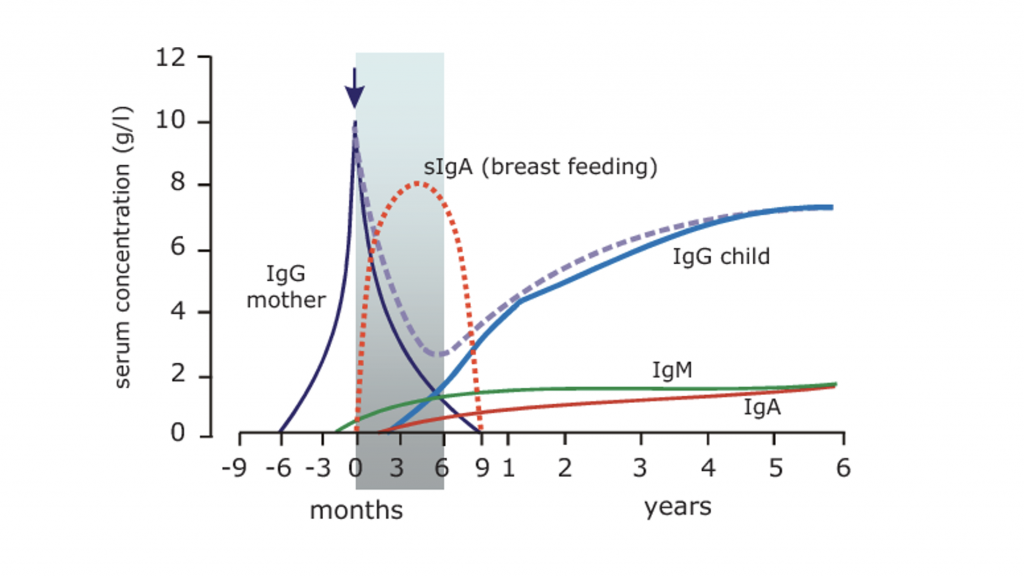
The rather complicated graph shows how the protection given by the mother to the baby before birth (called ‘IgG mother”) declines after birth. Immunoglobulins protect us all from infections. There are different types of immunoglobulins most commonly IgG, IgA, IgM and IgE. A mother is giving some of her immunoglobulin G [IgG] to her newborn baby through the placenta while the baby is in her womb. There is no more supply of IgG given from a mother to a baby after birth. However, an infant may get a booster of immunoglobulins from their mothers with IgA (sIgA) through breast milk.
Immunoglobulins [Igs] can be seen as one form of protection of humans from infections. It could be compared with a “police force (immunoglobulins) protecting us from intruders (infections)”.
In simple terms IgM is the immediate police force on the scene to deal with the intruders. IgG is the police force who remembers specific previous events and can mobilise ‘Ig M police’ very quickly if the “same intruders are detected again”. IgA is similar but “police” patrolling on outer surfaces such as the lining of the lungs or the bowel. IgA helps to fight chest infections and protect from gastroenteritis. The ‘IgM police force’ is trained and deployed to deal with infections from scratch if the body has never seen this infection before which takes a few days to be in full force. By then most infections have caused the body to show some symptoms like a runny nose, cough, fever and feeling unwell. The IgM police force is then building up and battling with the intruder (infection) and the illness will settle. It is important to understand that the ‘IgM police force’ is much faster deployed if there is any ‘IgG police’ around to recognise the intruders from a previous event and puts the ‘IgM police force’ together very fast. This is why many older children can deal with a lot of infections very well if they have come across it before and there is a lot of different IgG (background police).
So from 3 months onwards infants build up their own immunoglobulins (IgG, IgM and IgA). While they do this there is a real lack of defence mechanism which is most noticeable around 6 months and continues until school age. It is only after children meet most common viruses by contact with other sick children they learn how to fight it. We do also know that infections can be spread by asymptomatic adults or children who may not show any signs of illness but carry the virus. That is why your child may still get infections when at home and not in nursery or school.
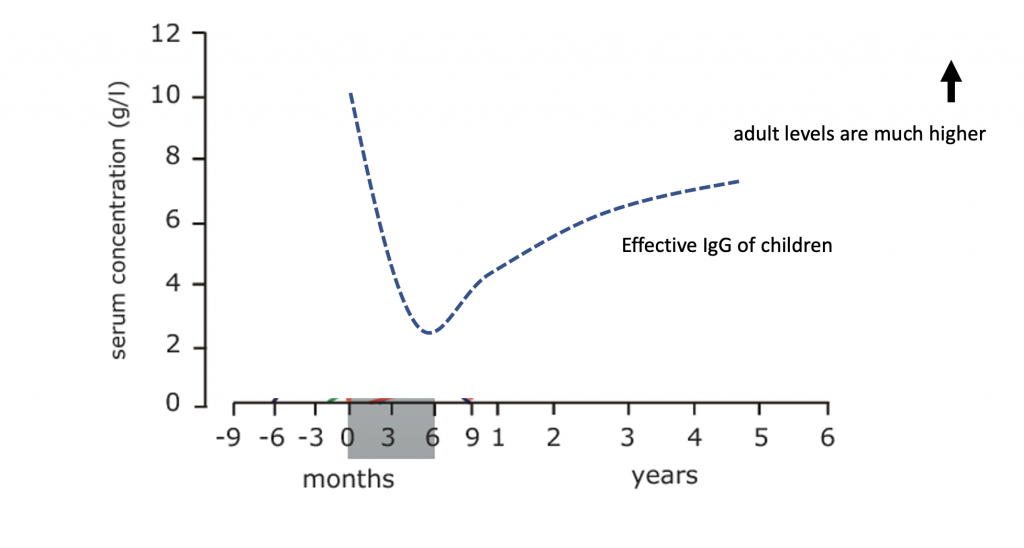
This is the combined level of all immunoglobulins of a small child from the previous graph and shows the actual level of protection a child has in the first 5 years of life. This is well ‘short’ of the average level of protection we as adults have. Hence it is normal for children to have many infections at that particular age.
Throughout our entire life, with every infection we add a little bit more to the immunoglobulins even when we tend to lose some over time.
A very important further concept is that the better we develop our immune system in childhood – the better we may be protected in old age and not develop secondary pneumonia after a common cold. In other words the more infections we fight as a child the longer we may live as an adult.
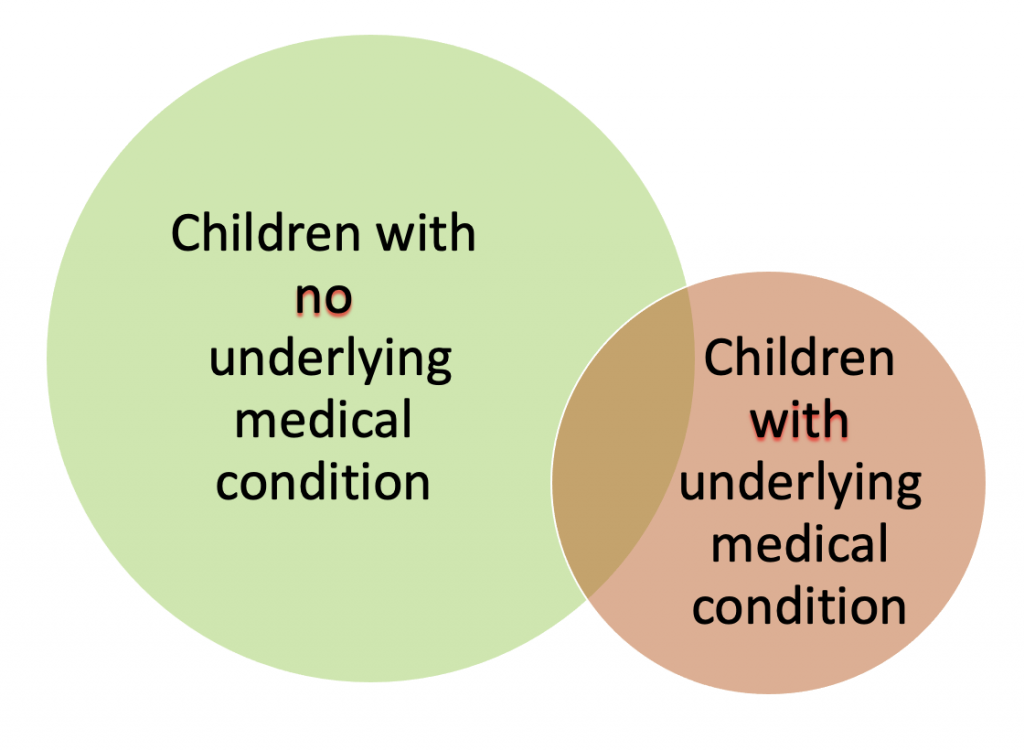
Life is never that easy. This is because it is never “black or white” – “right or wrong”!
If 95% of all healthy children have up to 12 infections lasting 3 weeks or less in a year it means that there are still 5% of healthy children who have even more infections.
On the other hand, children who do have “something wrong with them” may not even have 12 infections a year either.
There is obviously an overlap of healthy children with a lot of infections and ‘children who have something wrong with them’ and the same amount of infections.
This is why children with a lot of infections do need to be seen by a doctor and they need to be carefully assessed in order to work out whether to watch further or to arrange tests.
Your child should be at least seen face-to-face by your doctor and have a detailed history taken and a thorough examination. I would say that 70-90% of children I see do not have to have any further tests.
However, if your doctor opts for no tests at the time he or she should also offer a period of observation and therefore should arrange a review next time your child is ill or in 3 to 6 months latest.
There are many things that can be done to make a child better when they suffer from a viral infection. No remedy is an immediate cure but will contribute to make your child feel better and can boost a weakened immune system.
I have covered these remedies in a separate “Frequently Asked Questions”:
It is not possible to explain every possible condition in plain English here on this website but I will list most of those I usually exclude with history plus examination and/or further tests:
1) Environmental factors
2) Abnormalities of the lungs
3) Nutritional deficiencies
4) Recurrent viral wheezing and airborne triggers
5) Deficiencies of the immune system
6) Temporary lung conditions
7) Chronic lung conditions
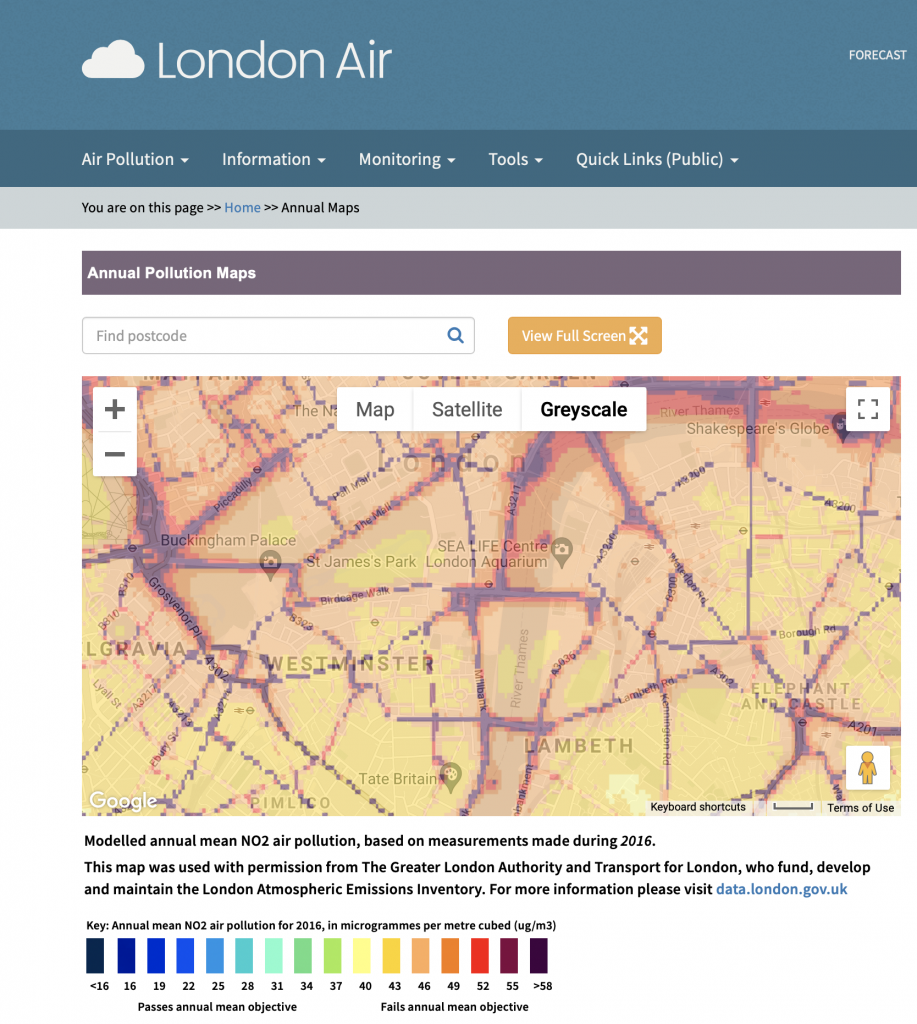
Air quality is increasingly recognised as a major contributing factors for acute and chronic respiratory illnesses. London Air is one of many websites where you can check your local air pollution and the air pollution where you may be outdoor on the way to shops or school.
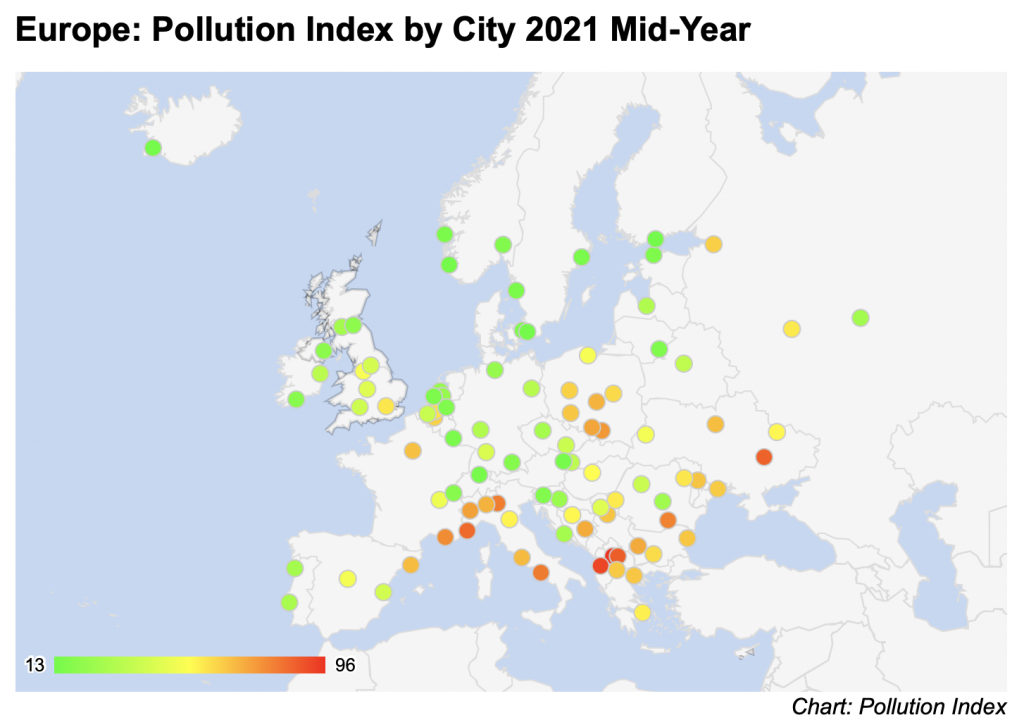
An overview how London compares in Europe and the rest of the world with regards to air quality can be found on www.numbeo.com.
What I find surprising after so many years of looking after children with chronic coughs and parental concerns, that many parents dismiss smoking or vaping indoor or outdoor as a contributing factor. Active and passive smoking is one of the best researched and understood contributing factors to recurrent lung problems in children but the most commonly given answer I hear is: “Yes I do/my partner does smoke but only outside…” or “..it is only vaping!”. In addition to the real risk of passive smoking, the risk of your child taking up smoking in adolescence if you as a parent smoke is also massively increased! (7)
Having said this, it is also relatively easy to point a finger at a member in the family who is smoking but actually supporting a smoker to help quitting is very hard for all involved. I have provided a link on my website on smoking cessation programmes but every family member needs to support those who are planning to kick the habit. On a positive note: quitting smoking is one of the health modifiers with the highest impact for oneself as well as the rest of the family and especially for a child.
7. Vuolo, M. & Staff, J. Parent and child cigarette use: a longitudinal, multigenerational study. Pediatrics 132, e568-577 (2013).
Other environmental factors such as mould, pet allergens and house dust are covered under allergic conditions.
A plain chest radiograph (x-ray) is often the first start if we order any tests.
There are many abnormalities which may affect recurrent infections which range from birth defects to accidental inhalation of food or toys to to other rare conditions.
I would check at least one chest x-ray after birth, which I usually order unless the child has had one before and it was normal. I may ask the parents or carer to organise the report or even the actual picture as I always prefer to see it with my own eyes rather than rely on a verbal report only. Modern x-ray machines use only a very low dose of radiation for a chest radiographs. Very few people know that a flight on an airplane for 2-3 hours or one extra day of naturally occurring background radiation exposes your child to the same amount of radiation as one chest x-ray!
In my experience, nutritional deficiencies are certainly a major contributor to recurrent infections. Many toddlers are not the best eaters when it comes to variety or the ‘green food’. In my practice, I come across iron and vitamin deficiencies very frequently. This weakens the immune system and the ability to fight infections well. Even when parents feel their children are eating well, a rapidly growing child may have far more needs for minerals and substances than parents expect. Multivitamins are often not given, given infrequently or not tolerated well by children and parents seem to think they are giving them more often than they actually do.
Nutritional deficiencies can be detected by simple blood tests and can be corrected quite easily. This has often a huge effect on a child’s performance but also infection rate.
Some children suffer form recurrent wheezy episodes or are sensitised to airborne allergens. Those children may not get more infections but tend to show more symptoms and their symptoms last for longer when they get a cold and cough. Hence the time of recovery between two episodes of them seem much shorter and they seem to be “constantly ill”.
There is usually a family history of hay fever or asthma, eczema and food allergies. While food allergies as such do not pre-dispose your child to infections their link to other illnesses such as asthma and hay fever. In some children it can be helpful to screen for a reaction sensitisation to airborne triggers such as mould, house dust mites, pets or outdoor allergens such as tree, grass or weed pollen.
Severe immunodeficiencies
While most parents are worried about severe immune deficiencies these become usually apparent in a very different way: Children with severe immunodeficiency usually have recurrent bacterial infections such as pneumonias, meningitis or deep skin infections typically starting before the age of 6 months. Bronchiolitis which is an infection which may occur before the age of 6 months is typically not an infection indicating a severe immune deficiency.
Mild immunodeficiencies
Children with recurrent viral infections form the age of 6 to 8 months onwards may have subtle immunodeficiencies and it is sometimes neccessasry to look for them. You can read more information about the conditions by clicking on them:
In most cases it is good to know about them although we do not necessarily use daily medication to treat your child for it. It is usually enough to look extra careful for potential bacterial infections when they are ill.
Some children with frequent viral infections develop a something like a “bacterial overgrowth”. This is typically a temporary condition but causes a self-perpetuating ongoing cough which typically lasts for 6 weeks or longer. This is called Protracted Bacterial Bronchitis or PBB. Click on the name to find separate parent information on this condition.
Some children may have a chronic lung condition and it is not possible to list all of them here. Such conditions are very rare and are often suspected by history and examination or obvious when doing a chest radiograph (chest x-ray) as part of the work up described above..
In some children special investigations are needed if they are suspected and will need to be explained by your doctor at the time. Routine screening at birth for cystic fibrosis makes it very unlikely now that your doctor will suspect this diagnosis but it is important to keep it in the mind when taking history and during examination.
This information is provided by Dr W Muller and will be regularly reviewed and updated.